From [MERCOLA] Data from Kansas show counties with mask mandates had a higher death rate than counties without a mask mandate; two other large studies found similar results, one that gathered data in Europe only and the other from 69 countries
According to a study in early 2021, face masks increase your daily inhalation of microplastics; another study released in April 2022 found microplastics similar to that used in face masks in lung tissue sampled during surgery. Some were found in the deepest parts of the lung
Data show that masks can collect antibiotic-resistant pathogens and trigger a cluster of symptoms called Mask-Induced Exhaustion Syndrome (MIES) that negatively impacts your immune system, and causes carbon dioxide retention, skin irritation, headaches, difficulty breathing and decreased cardiopulmonary capacity
It is crucial that accurate data are gathered and communicated to provide a strong foundation for developing local public policy before the next plandemic creates a scenario in which government officials attempt to mandate masking and lockdowns
Fiona Lashells is an 8-year-old second grader who lives in Florida. She made the local1 and national news2 when she was suspended an outrageous 38 times for standing up for her right to do something that isn't supported by data or science in a school system — wearing a mask.
The New York Post described Lashells as a “recalcitrant student,”3 who apparently knew and exercised her rights better than most. July 30, 2021, Florida Gov. Ron DeSantis4 issued an executive order ruling that school districts could not require students to wear masks. However, in defiance of authority, the Palm Beach County School District where Lashells lives reinstated their mask mandate.5
After DeSantis’s executive order was issued, Lashell's mom told her she didn't have to wear the mask for the upcoming school year. Lashell had been complaining about fatigue from wearing the mask during the last school year. At first, she was made to eat lunch alone in the hallway outside the office of an administrator. Soon, in-school suspensions began and were quickly followed by out-of-school suspensions.
After 38 suspensions, the school district repealed its mask mandate November 8, 2021. Out of the mouth of an 8-year-old came these words, “I’m not wearing a mask because you touch it, and you have germs on your hand. And then you put it on your face and breathe in all the germs.”6
Mandating masks for school children have been an unprecedented public move that has not been scientifically validated. Instead, CDC data7,8 show school children have the least risk from the virus and national data9 gathered before the pandemic show children who experience relational and social risks have a four times higher likelihood of having mental, emotional or behavioral problems.
In other words, the government mandated masks on a population who had the least risk of illness and the greatest long-term risk from wearing the mask. Several journals have finally begun publishing data gathered during the pandemic revealing that while prevention efficacy is minimal or not evident,10 wearing masks increases your risk of death if you do get sick.11
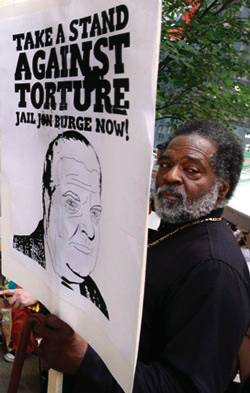
Death Rate Rises in Counties With Mask Mandate
German physician Dr. Zacharias Fögen12 found no published evidence that masking could effectively reduce the severity of the disease or had an influence on case fatality.
Fögen used demographic data from the state of Kansas to run an analysis on a county-wide level comparing counties that mandated mask-wearing and those that didn't. The data suggested that using a mask could present a greater threat to the user, making it a “debatable epidemiological intervention.”13
The death rate in counties where masks were mandated was higher by 85%. After an analysis that accounted for confounding factors, the mortality rate remained 52% higher in counties that mandated masking.
Further analysis showed that 95% of the effect “can only be attributed to COVID-19, so it is not CO2, bacteria or fungi under the mask.”14 In other words, while the pathogens or CO2 buildup may have weakened the immune system, it was COVID-19 that caused the deaths.
He named this the “Foegen Effect,” referring to the reinhalation of viral particles trapped in droplets and deposited on the mask, which worsens outcomes. In the journal article, he writes:15
“The most important finding from this study is that contrary to the accepted thought that fewer people are dying because infection rates are reduced by masks, this was not the case. Results from this study strongly suggest that mask mandates actually caused about 1.5 times the number of deaths or ~50% more deaths compared to no mask mandates.
The mask mandates themselves have increased the CFR (case fatality rate) by 1.85 / 1.58 or by 85% / 58% in counties with mask mandates. It was also found that almost all of these additional deaths were attributed solely to COVID-19.
This study revealed that wearing facemasks might impose a great risk on individuals, which would not be mitigated by a reduction in the infection rate. The use of facemasks, therefore, might be unfit, if not contraindicated, as an epidemiologic intervention against COVID-19.”
Fögen notes two other large studies that found similar results with case fatality rates. The first was published in the journal Cureus16 and found no association between case numbers and mask compliance in Europe but a positive association with death and mask compliance.
The second study17 was published in PLOS One and demonstrated there was an association between negative COVID outcomes and mask mandates across 847,000 people in 69 countries.
Masking Increases Other Health Risks
These conclusions were similar to those reached in a preprint study18 posted August 7, 2021, that challenged the prevailing belief masking could slow the spread of the virus. They found mask-wearing could:
Promote facial alkalinization
Encourage dehydration, which enhances barrier breakdown and raises the risk of bacterial infection
Increase headaches and sweating
Decrease cognitive precision, which can lead to medical errors
Many of the mask mandates were initiated to stay in line with CDC guidelines at the time. The data were gathered over multiple seasons using information the CDC gathered, from which the researchers originally concluded, “Mask mandates and use are not associated with slower state-level COVID-19 spread during COVID-19 growth surges.”19 They subsequently revised the paper and wrote:20
“The sudden onset of COVID-19 compelled adoption of mask mandates before efficacy could be evaluated. Our findings do not support the hypothesis that greater public mask use decreases COVID-19 spread. As masks have been required in many settings, it is prudent to weigh potential benefits with harms. Masks may promote social cohesion during a pandemic, but risk compensation can also occur.”
According to a study by Chinese scientists posted in January 2021, wearing a face mask can increase your daily inhalation of microplastics.21 In April 2022,22 a team of scientists from Hull York Medical School published findings that showed 39 microplastic particles in 11 of 13 lung tissues sampled during lung surgery.
According to the lead author, microplastics have been found in autopsies in the past, but this is the first study to demonstrate they are found in the living. Interestingly, these microparticles were also found in the lowest parts of the lungs, which researchers had once thought they could not possibly reach.23
The study authors found the subjects had 12 types of microplastics and the most abundant were polypropylene (PP) and polyethylene terephthalate (PET).24 This finding points to the recent ubiquitous use of blue surgical masks during the pandemic as PP is the most used plastic component in those masks.
Expert Says COVID Face Coverings Are Not Masks
One 2021 study25 looked at the risks of wearing blue surgical face masks and inhaling microplastics. The researchers found that reusing masks could increase the risk of inhaling microplastic particles and that N95 respirators had the lowest number of microplastics released when compared to not wearing a mask.
They wrote, “Surgical, cotton, fashion and activated carbon masks wearing pose higher fiber-like microplastic inhalation risk …”26 And yet, according to Chris Schaefer, a respirator specialist and training expert, what health experts have been calling masks are not really masks at all.27
Schaefer calls these “breathing barriers” as they “don't meet the legal definition” of a mask. He was emphatic that the surgical masks used by consumers throughout Canada, the U.S. and the world are shedding microplastics small enough to be inhaled.28
“A [proper] mask has engineered breathing openings in front of the mouth and nose to ensure easy and effortless breathing. A breathing barrier is closed both over the mouth and nose. And by doing that, it captures carbon dioxide that you exhale, forces you to re-inhale it, causing a reduction in your inhaled oxygen levels and causes excessive carbon dioxide. So, they’re not safe to wear.”
He encourages people to cut one open and look at the loose fibers that are easily dislodged within the product.29
“The heat and moisture that it captures will cause the degradation of those fibres to break down smaller. Absolutely, people are inhaling [microplastic particles]. I’ve written very extensively on the hazards of these breathing barriers the last two years, I’ve spoken to scientists [and other] people for the last two years about people inhaling the fibres.
If you get the sensation that you’ve gotten a little bit of cat hair, or any type of irritation in the back of your throat after wearing them. That means you’re inhaling the fibres.”
He went on to note that anyone exposed to these types of fibers in an occupational setting would be required to wear protection. Instead, people are using products that increase the risk of inhaling fibers that "break down very small and, well, what that’s going to do to people in the form of lung function — as well as toxicity overload in their body — I guess we’ll know in a few years."30
Mask Policy Influenced by Two Hair Stylists, Not Science
In the early days of the pandemic, there was a rush on masks, causing supplies for health care practitioners to dwindle. At the time, health officials were adamant that people should NOT wear masks. In February 2020, Christine Francis, a consultant for infection prevention and control at the World Health Organization, said, “Medical masks … cannot protect against the new coronavirus when used alone … WHO only recommends the use of masks in specific cases.”31
Those specific cases include if you had a cough, fever or difficulty breathing. In other words, you should wear them only if you’re actively sick and showing symptoms. “If you do not have these symptoms, you do not have to wear masks because there is no evidence that they protect people who are not sick,” she continued.32
Also in February 2020, U.K. health authorities advised against the use of masks, even for people working in community or residential care facilities.33 In March 2020, U.S. Surgeon General Jerome Adams publicly agreed, tweeting a message stating, “Seriously people- STOP BUYING MASKS!” and going on to say that they are not effective in preventing the general public from catching coronavirus.34
Fast forward one year and CDC’s mask policy appears to have been determined solely on observational studies, not randomized controlled trials (RCTs) that are the gold standard in science.
“In general, observational studies are not only of lower quality than RCTs but also are more likely to be politicized, as they can inject the researcher’s judgment more prominently into the inquiry and lend themselves, far more than RCTs, to finding what one wants to find,” explained Jeffrey Anderson, former director of the Bureau of Justice Statistics, in a review published by City Journal.35
The CDC has relied on an observational cohort study published in July 2020, of two hair stylists from a Missouri beauty salon.36 The stylists tested positive for COVID-19, developed symptoms, but continued to see 139 clients until they received the positive test. They and their clients wore masks during this time.
The data showed that 67 of the clients tested negative and the other 72 did not report symptoms. From this, the CDC concluded that the “face covering policy likely mitigated the spread of SARS-CoV-2.”37
Anderson explained the study had major limitations, “The apparent lack of spread of COVID-19 could have been a result of good ventilation, good hand hygiene, minimal coughing by the stylists, or the fact that stylists generally, as the researchers note, ‘cut hair while clients are facing away from them.’”38
Another important limiting factor is the lack of a control group. Would the results have been different if the stylists or the clients were not wearing masks? No one knows. But what has become apparent is the consistent lack of quality in studies and information on which public policy has been based since the start of the pandemic.
Antibiotic-Resistant Pathogens and Mask Exhaustion Syndrome
The featured study looked only at the raw numbers from Kansas and did not delve into what may have been behind the increasing severity of disease and death in the people who wore masks.
For example, when researchers from the University of Antwerp, Belgium, analyzed the microbial community on surgical and cotton face masks from 13 healthy volunteers after being worn for four hours, bacteria including Bacillus, Staphylococcus and Acinetobacter were found — 43% of which were antibiotic-resistant.39
Researchers from Germany similarly questioned whether a mask that covers your nose and mouth is “free from undesirable side effects” and potential hazards in everyday use.40 It turned out they were not and instead posed significant adverse effects and pathophysiological changes, including the following, which often occur in combination:41
This cluster of symptoms is referred to as Mask-Induced Exhaustion Syndrome (MIES).42 The researchers warned that people who are sick, suffering from certain chronic conditions, pregnant women and children may be at particular risk from extended mask-wearing. Short-term effects may include microbiological contamination, exhaustion, headaches, carbon dioxide retention and skin irritation.
However, long-term effects can lead to chronic issues triggered by “a chronic sympathetic stress response induced by blood gas modifications and controlled by brain centers. This in turn induces and triggers immune suppression and metabolic syndrome with cardiovascular and neurological diseases.”43
Research is needed to determine if the severity of disease and increased death rates in those who wear masks is related to the antibiotic-resistant bacteria that collect on the masks, the impact MIES has on your immune system and the potential dehydration chronic mask wearers may experience, or something else.
Accurate data must be gathered and communicated to provide a strong foundation for developing local public policy before the next plandemic creates a scenario in which government officials attempt to mandate masking and lockdowns — again.
- Sources and References
1 ABC News10, November 8, 2021
2, 3 New York Post, November 3, 2021
4 Flgov.com, Ron Desantis July 30, 2021
5 The Daily Wire, November 14, 2021
6 The Daily Wire, November 14, 2021, para 6
7 Centers for Disease Control and Prevention, June 2, 2022
8 Centers for Disease Control and Prevention, June 6, 2022, Table 1 Total tab
9 Johns Hopkins Bloomberg School of Public Health, January 25, 2022
10, 20 medRxiv, August 7, 2021, doi.org/10.1101/2021.05.18.21257385
11, 12, 13, 15 Medicine, 2022;101(7)
14 The Daily Skeptic, May 2, 2022
16 Cureus, 2022;14(4)
17 PLOS|One, 2021, doi.org/10.1371/journal.pone.0252315
18 medRxiv, August 7, 2021, doi.org/10.1101/2021.05.18.21257385 Abstract
19 medRxiv, May 25, 2021; doi.org/10.1101/2021.05.18.21257385
21 Yahoo News, January 1, 2021
22, 23 Hull York Medical School, April 6, 2022
24, 27, 28, 29, 30 Western Standard, April 17, 2022
25, 26 Journal of Hazardous Material, 2021;411
31, 32 BitChute January 1, 2021 1:58
33, 34, 35, 38 City Journal August 11, 2021
36, 37 MMWR July 17, 2020 / 69(28);930-932
39 Frontiers in Medicine, 2021; doi.org/10.3389/fmed.2021.732047
40, 41, 42, 43 International Journal of Environmental Research and Public Health, 2021 Apr; 18(8): 4344