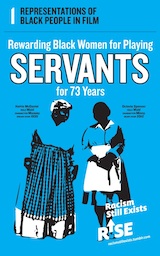
Due to Racism, Black Women [w/Grad/Doctorate Degrees] 3x More Likely to Die After Giving Birth than White Women [w/o high school degrees]
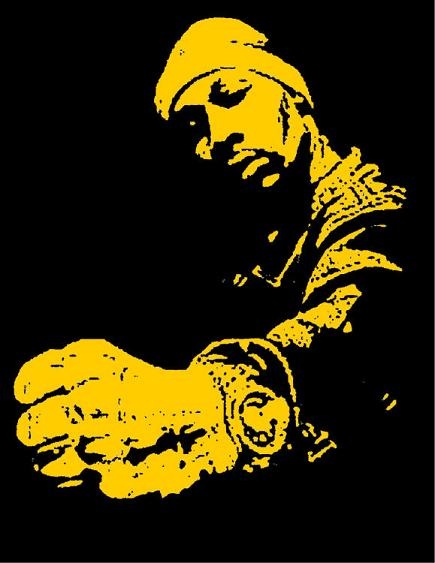
/From [NPR] On a melancholy Saturday this past February, Shalon Irving's "village" — the friends and family she had assembled to support her as a single mother — gathered at a funeral home in a prosperous black neighborhood in southwest Atlanta to say goodbye.
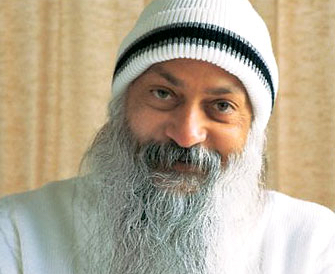
The afternoon light was gray but bright, flooding through tall, arched windows and pouring past white columns, illuminating the flag that covered her casket. Sprays of callas and roses dotted the room like giant corsages, flanking photos from happier times: Shalon in a slinky maternity dress, sprawled across her couch with her puppy; Shalon, sleepy-eyed and cradling the tiny head of her newborn daughter, Soleil. In one portrait, Shalon wore a vibrant smile and the crisp uniform of the Commissioned Corps of the U.S. Public Health Service, where she had been a lieutenant commander. Many of the mourners were similarly attired. Shalon's father, Samuel, surveyed the rows of somber faces from the lectern. "I've never been in a room with so many doctors," he marveled. "... I've never seen so many Ph.D.s."
At 36, Shalon had been part of their elite ranks — an epidemiologist at the Centers for Disease Control and Prevention, the pre-eminent public health institution in the U.S. There she had focused on trying to understand how structural inequality, trauma and violence made people sick. "She wanted to expose how people's limited health options were leading to poor health outcomes," said Rashid Njai, her mentor at the agency. "To kind of uncover and undo the victim-blaming that sometimes happens where it's like, 'Poor people don't care about their health.' " Her Twitter bio declared: "I see inequity wherever it exists, call it by name, and work to eliminate it."
Much of Shalon's research had focused on how childhood experiences affect health later on — examining how kids' lives went off track, searching for ways to make them more resilient. Her discovery in mid-2016 that she was pregnant with her first child had been unexpected and thrilling.
Then the unthinkable happened. Three weeks after giving birth, Shalon collapsed and died from complications of high blood pressure.
The researcher working to eradicate disparities in health access and outcomes had become a symbol of one of the most troublesome health disparities facing black women in the U.S. today: disproportionately high rates of maternal mortality. The main federal agency seeking to understand why so many American women — especially black women — die, or nearly die from complications of pregnancy and childbirth had lost one of its own.
Even Shalon's many advantages — her B.A. in sociology, her two master's degrees and dual-subject Ph.D., her gold-plated insurance and rock-solid support system — had not been enough to ensure her survival. If a village this powerful hadn't been able to protect her, was any black woman safe?
The sadness in the chapel was crushing. Shalon's long-divorced parents had already buried both their sons; she had been their last remaining child. Wanda Irving had been especially close to her daughter — role model, traveling companion, emotional touchstone. She sat in the front row in a black suit and veiled hat, her face a portrait of unfathomable grief. Sometimes she held Soleil, fussing with her pink blanket. Sometimes Samuel held Soleil, or one of Shalon's friends.
A few of Shalon's villagers rose to pay tribute; others sat quietly, poring through their funeral programs. Daniel Sellers, Shalon's cousin from Ohio and the baby's godfather, spoke for all of them when he promised Wanda that she would not have to raise her only grandchild alone.
"People say to me, 'She won't know her mother.' That's not true," Sellers said. "Her mother is in each and every one of you, each and every one of us. ... This child is a gift to us. When you remember this child, you remember the love that God has pushed down through her for all of us. Soleil is our gift."
The memorial service drew to a close, the bugle strains of taps as plaintive as a howl. Two members of the U.S. Honor Guard removed the flag from Shalon's coffin and held it aloft. Then they folded it into a precise triangle small enough for Wanda and Samuel to hold next to their hearts.
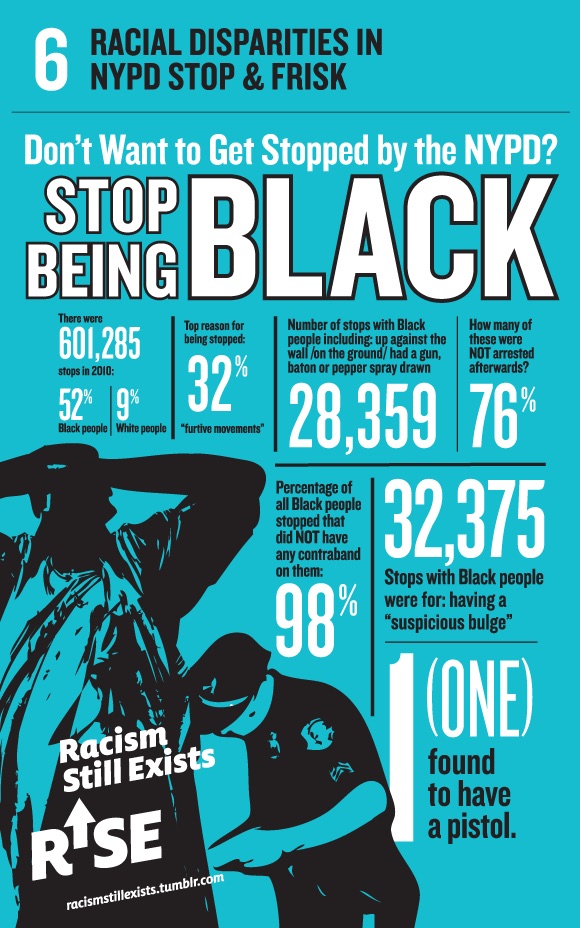
Racial disparity across incomes
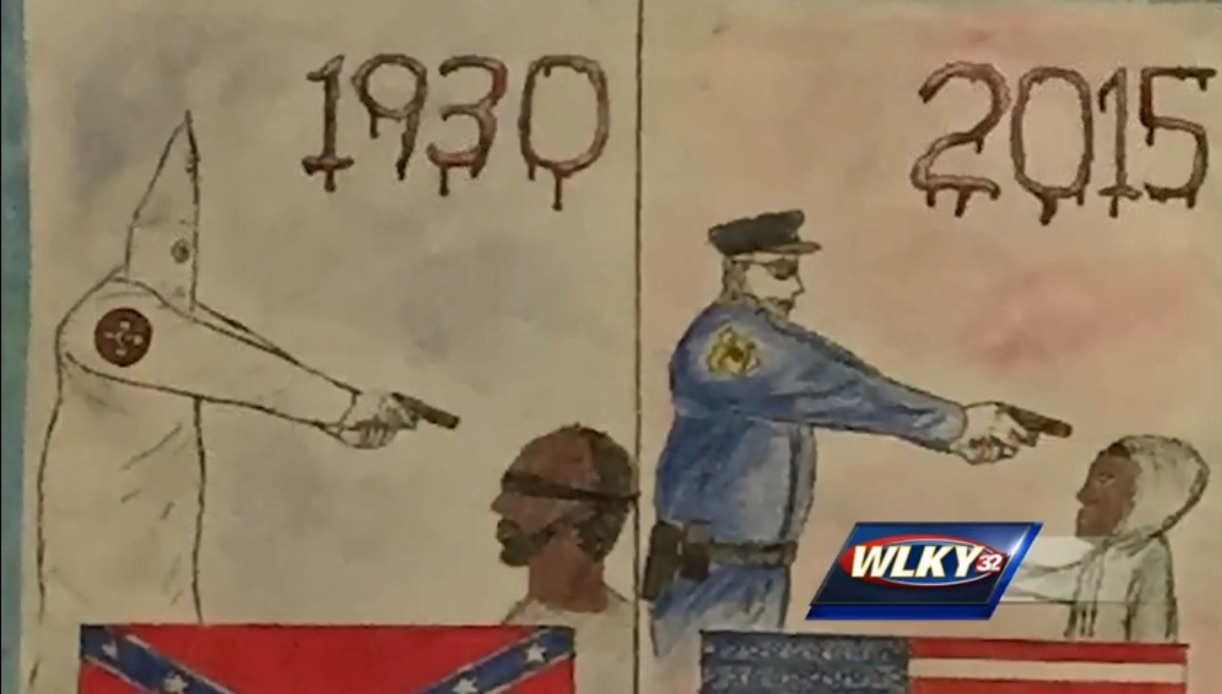
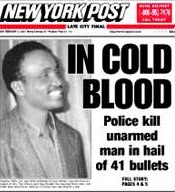
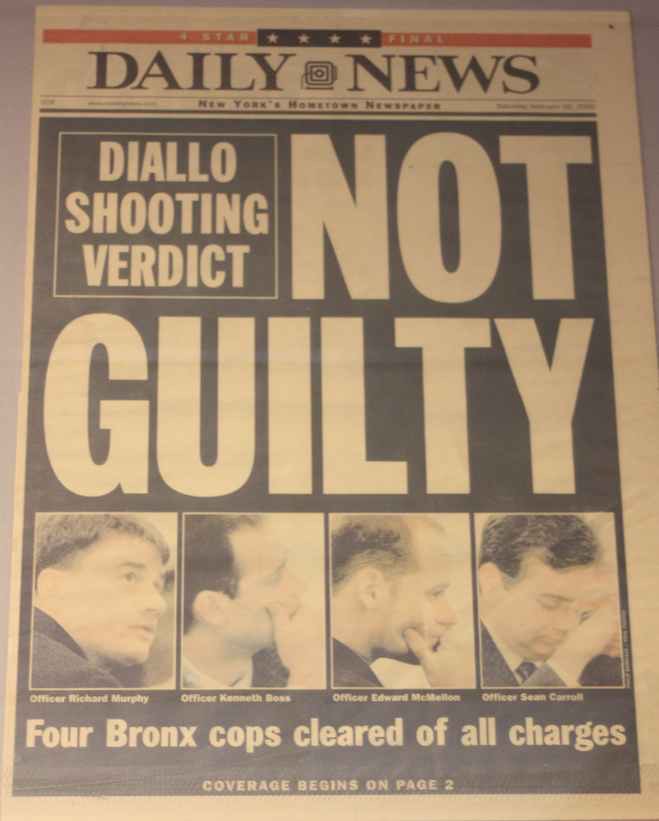
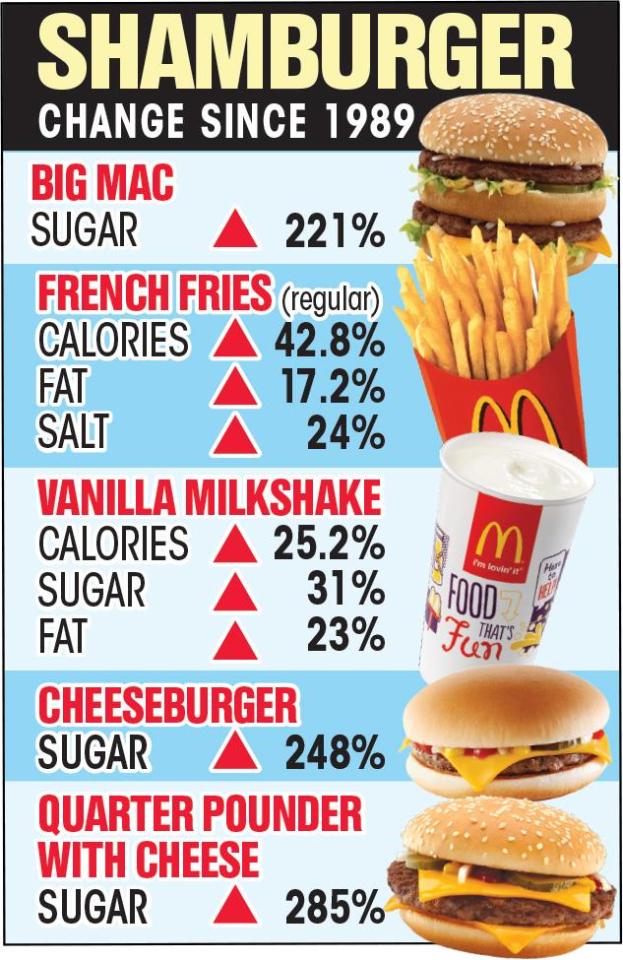
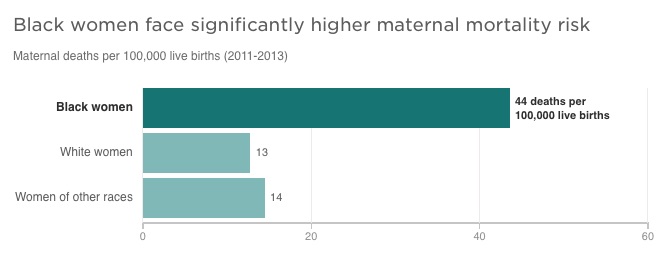
In recent years, as high rates of maternal mortality in the U.S. have alarmed researchers, one statistic has been especially concerning. According to the CDC, black mothers in the U.S. die at three to four times the rate of white mothers, one of the widest of all racial disparities in women's health. Put another way, a black woman is 22 percent more likely to die from heart disease than a white woman, 71 percent more likely to perish from cervical cancer, but 300 percent more likely to die from pregnancy- or childbirth-related causes. In a national study of five medical complications that are common causes of maternal death and injury, black women were two to three times more likely to die than white women who had the same condition.
That imbalance has persisted for decades, and in some places, it continues to grow. In New York City, for example, black mothers are 12 times more likely to die than white mothers, according to the most recent data; in 2001-2005, their risk of death was seven times higher. Researchers say that widening gap reflects a dramatic improvement for white women but not for blacks.
The disproportionate toll on African-Americans is the main reason the U.S. maternal mortality rate is so much higher than that of other affluent countries. Black expectant and new mothers in the U.S. die at about the same rate as women in countries such as Mexico and Uzbekistan, the World Health Organization estimates.
What's more, even relatively well-off black women like Shalon Irving die and nearly die at higher rates than whites. Again, New York City offers a startling example: A 2016 analysis of five years of data found that black, college-educated mothers who gave birth in local hospitals were more likely to suffer severe complications of pregnancy or childbirth than white women who never graduated from high school.
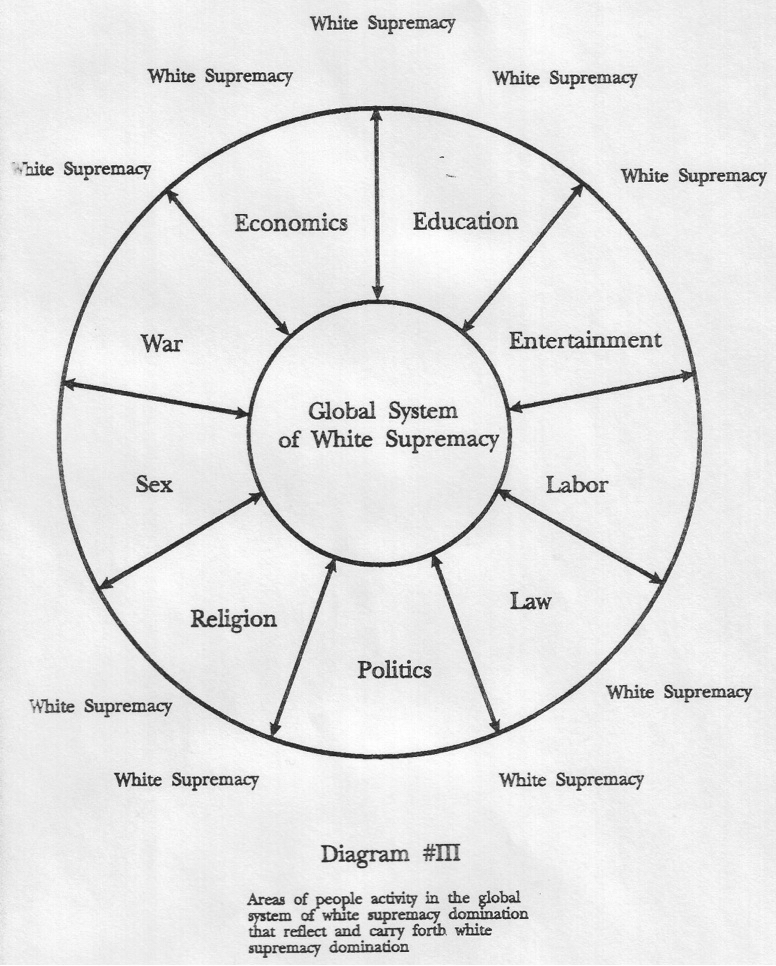
The fact that someone with Shalon's social and economic advantages is at higher risk highlights how profound the inequities really are, said Raegan McDonald-Mosley, the chief medical director for Planned Parenthood Federation of America, who met her in graduate school at Johns Hopkins University and was one of her closest friends. "It tells you that you can't educate your way out of this problem. You can't health care-access your way out of this problem. There's something inherently wrong with the system that's not valuing the lives of black women equally to white women." [what is racism/white supremacy?]
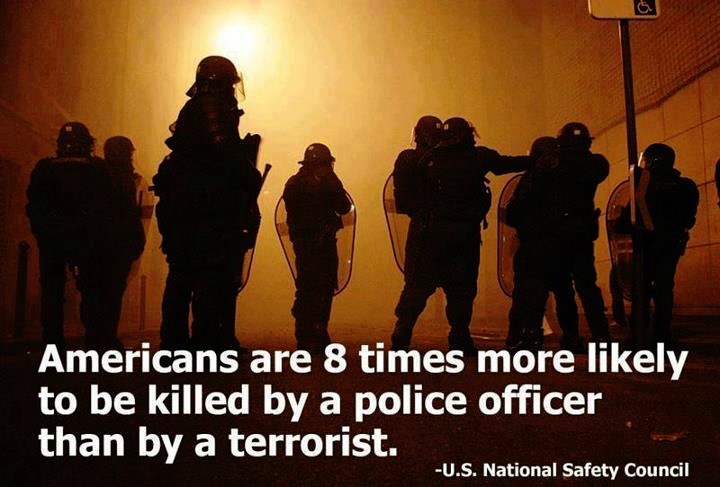
For much of American history, these types of disparities were largely blamed on blacks' supposed susceptibility to illness — their "mass of imperfections," as one doctor wrote in 1903 — and their own behavior. But now many social scientists and medical researchers agree, the problem isn't race but racism.
The systemic problems start with the type of social inequities that Shalon studied — differing access to healthy food and safe drinking water, safe neighborhoods and good schools, decent jobs and reliable transportation.
Black women are more likely to be uninsured outside of pregnancy, when Medicaid kicks in, and thus more likely to start prenatal care later and to lose coverage in the postpartum period. They are more likely to have chronic conditions such as obesity, diabetes and hypertension that make having a baby more dangerous. The hospitals where they give birth are often the products of historical segregation, lower in quality than those where white mothers deliver, with significantly higher rates of life-threatening complications.
Those problems are amplified by unconscious biases that are embedded in the medical system, affecting quality of care in stark and subtle ways. In the more than 200 stories of African-American mothers that ProPublica and NPR have collected over the past year, the feeling of being devalued and disrespected by medical providers was a constant theme.
There was the new mother in Nebraska with a history of hypertension who couldn't get her doctors to believe she was having a heart attack until she had another one. The young Florida mother-to-be whose breathing problems were blamed on obesity when in fact her lungs were filling with fluid and her heart was failing. The Arizona mother whose anesthesiologist assumed she smoked marijuana because of the way she did her hair. The Chicago-area businesswoman with a high-risk pregnancy who was so upset at her doctor's attitude that she changed OB/GYNs in her seventh month, only to suffer a fatal postpartum stroke. [MORE]