How Racism Creeps Into Medicine The history of a medical instrument reveals the dubious science of racial difference.
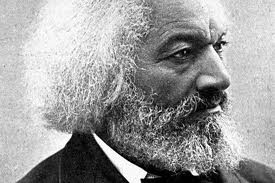
/In 1864, the year before the Civil War ended, a massive study was launched to quantify the bodies of Union soldiers. One key finding in what would become a 613-page report was that soldiers classified as "White" had a higher lung capacity than those labeled "Full Blacks" or "Mulattoes." The study relied on the spirometer—a medical instrument that measures lung capacity. This device was previously used by plantation physicians to show that black slaves had weaker lungs than white citizens. The Civil War study seemed to validate this view. As early as Thomas Jefferson’s Notes on the State of Virginia, in which he remarked on the dysfunction of the “pulmonary apparatus” of blacks, lungs were used as a marker of difference, a sign that black bodies were fit for the field and little else. (Forced labor was seen as a way to “vitalize the blood” of flawed black physiology. By this logic, slavery is what kept black bodies alive.)
The notion that people of color have a racially defined deficiency isn't new. The 19th century practice of measuring skulls, and equating them with morality and intelligence, is perhaps the most infamous example. But race-based measurements still persist. Today, doctors examine our lungs using spirometers that are "race corrected." Normal values for lung health are reduced for patients that doctors identify as black. Not only might this practice mask economic or environmental explanations for lower lung capacity, but the logic of innate, racial difference is built into things like disability estimates, pre-employment physicals, and clinical diagnoses that rely on the spirometer. Race has become a biologically distinct, scientifically valid category despite the unnatural and social process of its creation.
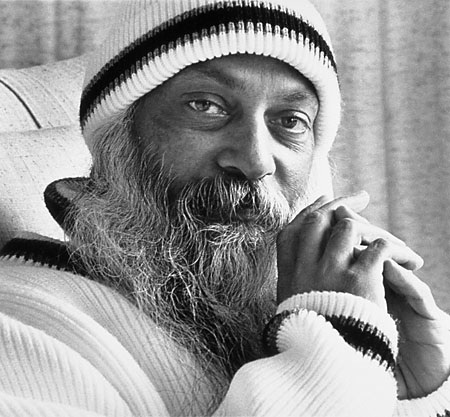
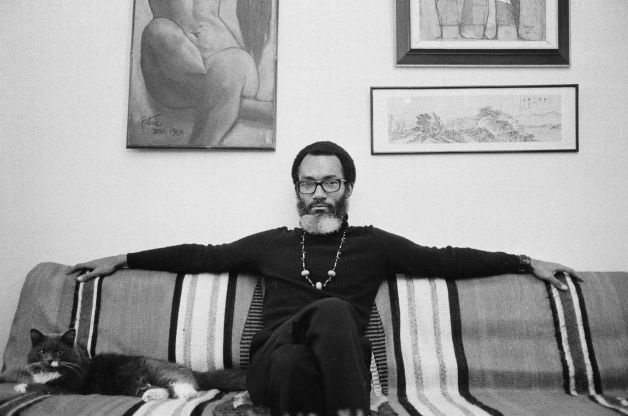
In her recent book Breathing Race into the Machine, Lundy Braun, a professor of Africana studies and medical science at Brown University, reveals the political and social influences that constantly shape science and technology. She traces the history of the spirometer and explains its role in establishing a hierarchy of human health, and the belief that race is a kind of genetic essence. I spoke with her about the science of racial difference, its history, and its resurgence.
Hamza Shaban: How did the idea of race corrections and differing lung capacity come about?
Lundy Braun: My research suggests that Samuel Cartwright, a Southern physician and plantation owner, was the first person to use the spirometer to compare lung capacity in blacks and whites. The first major study making racial comparisons of lung capacity with a large sample size was the anthropometric study of Union soldiers directed by Benjamin Apthorp Gould, published in 1869.
The idea about the pathology of black lungs circulated in medical groups in the late 19th century but the next scientifically modern racial comparison was published in the Journal of the American Medical Association in 1922. This paper was followed by a flurry of studies in the 1920s, some of which continue to be cited in the 2000s. Gould's book also continues to be cited.
Shaban: So within the medical community this is a well-established concept?
Braun: If you look at the scientific literature, virtually everyone in the world has lower lung capacity than people classified as whites. There is a scientific consensus. The question I’m interested in is: How did this idea of difference get into science? And how was difference explained? The problem here is the survival of the framework of innate racial difference.
Shaban: Race correction is actually built into the spirometer, right?
Braun: When I interviewed physicians they were sort of vaguely aware of race correction. But they don’t necessarily know that they’re activating a correction factor when they push the button or select a certain drop-down menu. Some even argued that they didn’t race correct, interestingly enough, but when I looked at the specification sheet, a correction factor was built into the machine.
Shaban: When a patient goes to see their doctor about their lungs, how does the doctor racially classify their patient?
Braun: In my interviews I asked physicians how they assessed race. I got a variety of responses. Many said they just "eyeballed" it—and never asked the individual any questions about their race. Others asked people to self-identify. But it can be awkward to ask someone their race for a lung function test. Patients might wonder why race is relevant for this particular test. So, in general, my research suggests that operators/clinicians simply guess a patient's race based on the usual simplistic physical characteristics historically associated with "race," like skin color—a poor marker for race globally. This guess may have little to do with how someone self-identifies or the richness of their ancestry. [MORE]