The high price of racial health disparities
/Reducing racial health disparities will take more than providing additional services in poor neighborhoods; it also requires confronting inequality and empowering communities
Why do some people get sicker and die sooner than others? The answer involves more than our genes, behaviors and medical care, according to a new study by the Joint Center for Political and Economic Studies and the advocacy group Equity Inc. It turns out that where we live is often the strongest predictor of our well-being, and that disparities along racial and class lines in health outcomes and access to care mirror the inequities in every other aspect of people's lives.
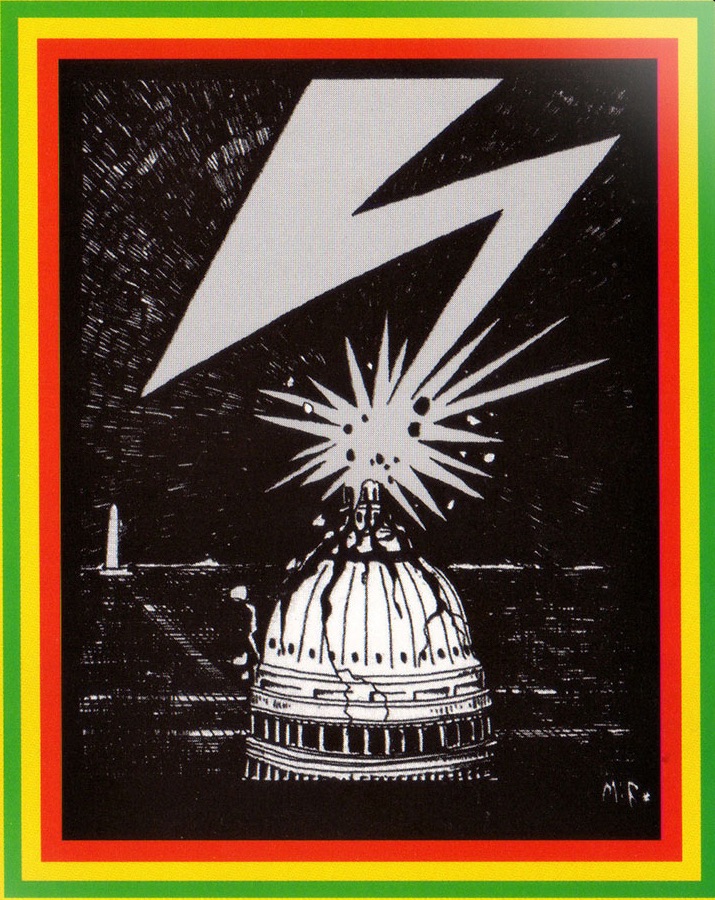
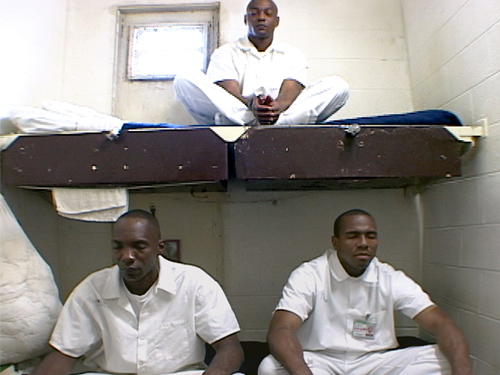
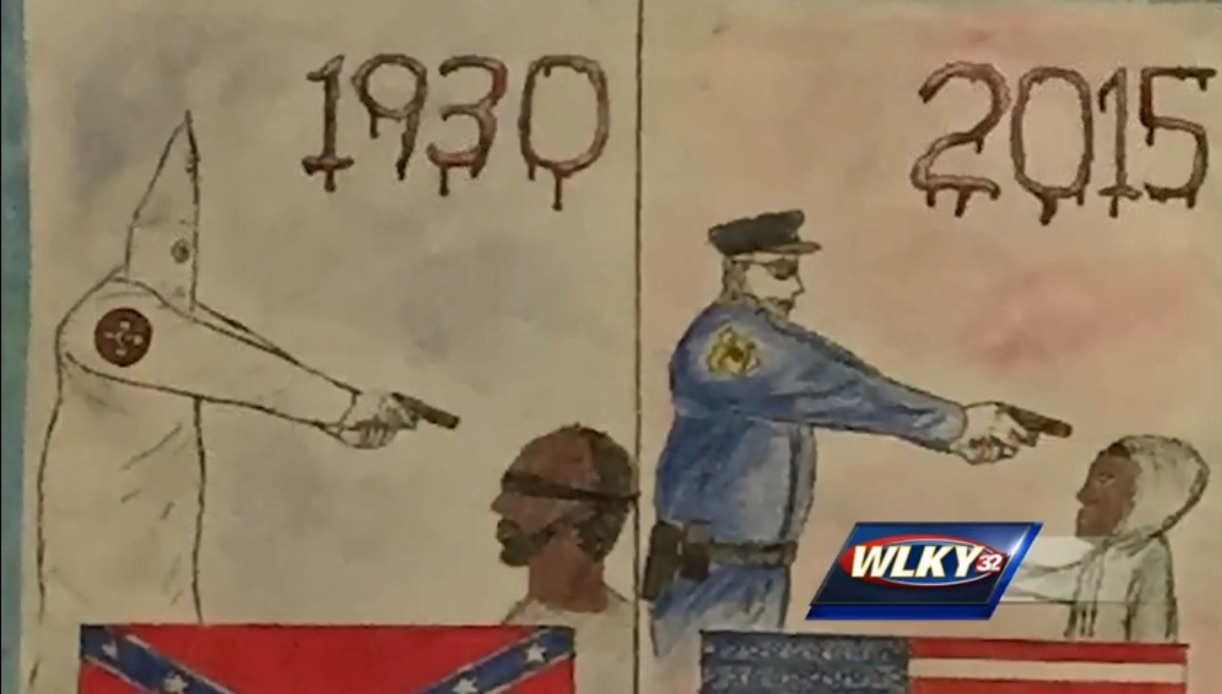
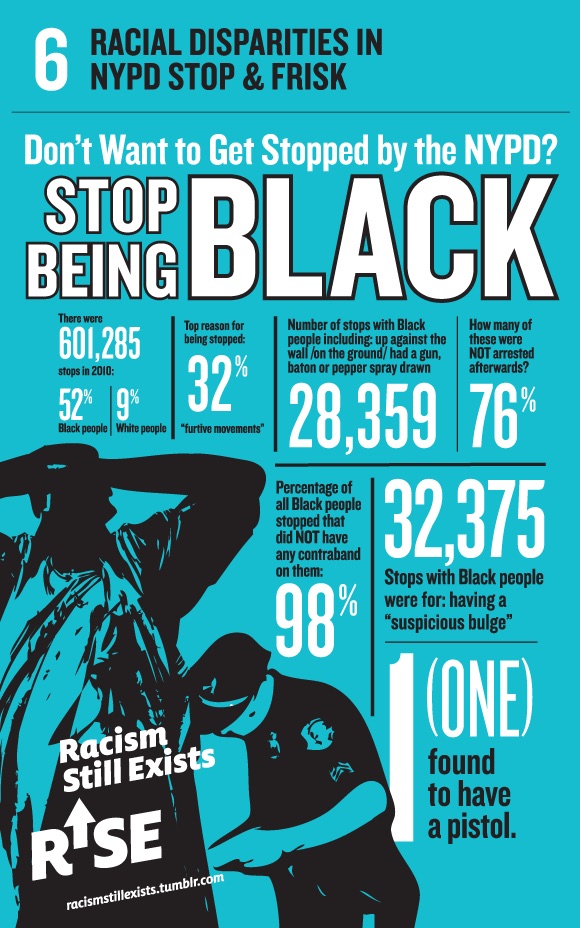
The report's findings confirm earlier studies that have shown persistently large gaps in health outcomes between different areas of the country, the state and even parts of the same city. In Baltimore, for example, residents of poor, largely African-American communities are known to suffer far higher rates of infant and child mortality, premature death and chronic illness than those of affluent, largely white neighborhoods elsewhere in the city.
Average life expectancy for affluent, white residents in Roland Park, for example, is nearly 30 years longer than for poor, African-American residents in Upton/Druid Heights. Meanwhile, the infant mortality rate among black women in some city neighborhoods is three or four times the state average. By almost any measure — including hospital visits for chronic conditions such as hypertension, diabetes and asthma — place matters even more than access to care as the most important determinant of people's health and well-being.
Recognizing the urgency of producing better health outcomes for poor and minority residents, Maryland has encouraged the creation of so-called health enterprise zones in areas around the state where the disparities are greatest. The enterprise zones would offer tax incentives for doctors, hospitals, business groups, churches and community associations to form public-private partnerships that provide additional medical and support services to underserved communities.
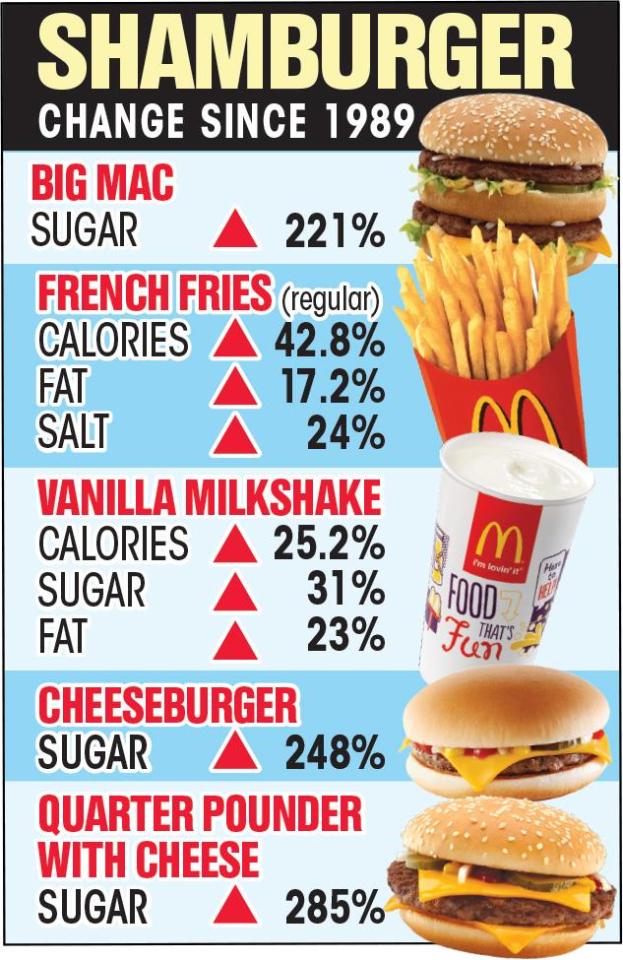
Last week, a number of such partnerships submitted applications for state grants that would allow them to set up pilot projects in parts of East and Northwest Baltimore. Their mission will be not only to promote greater access to primary medical care so that people don't wait until they are so sick they have to visit a hospital emergency room, but also to offer information and instructional programs that encourage residents to get more physical exercise, eat healthier foods, watch their weight and cut back on alcohol and tobacco use.
Yet simply providing better care and opportunities for a healthier life style won't by themselves close the gap in health outcomes based on race and class. One of the most important insights of the Joint Center report is that it isn't enough to simply parachute additional services into a marginalized community that has been demoralized by decades of social disorganization and neglect. People won't respond to the best-intentioned help from outsiders unless they feel empowered to take control of their own destinies and create a better future for themselves.
That is why organizing poor communities to address all the issues confronting them must be at the heart of any effort to reduce race- and class-based disparities in health outcomes. The community health workers who provide the link between medical service providers and local residents need to step beyond their role as health care professionals. They must become leaders who can mobilize their neighbors to demand a say in all the important decisions that affect the welfare of their communities, from education and public safety to zoning regulations and environmental protection.
That's a tall order for health workers who will be given only a brief training period before they are sent out into their communities to forge relationships between neighborhood residents and the health care partnerships that provide primary medical care and support services. Most of them will live in the communities they serve; research has shown that such partnerships are more sustainable when they employ local residents who have a personal stake in improving the quality of life in the place they call home. And the payoff is enormous if they succeed, because we pay a huge price for the inequalities in health outcomes that are generated along racial and class lines.
In just the three years between 2003 and 2006, Johns Hopkins and University of Maryland researchers found, racial health disparities cost the nation $230 billion in direct medical costs. That's three quarters of a trillion dollars in additional costs over a decade, money that otherwise could have been used to build schools, repair roads and bridges or hire more police, firefighters and emergency medical personnel.
Empowering communities to reduce those disparities also empowers them to tackle the conditions that create them, because the health outcomes in communities are affected not just by the number of doctors, clinics and hospitals operating there but by the totality of the social, economic and physical environments in which people live and work. The gap in health outcomes is as much a function of the inequities in the rest of people's lives as it is of unequal access to care. And the solution lies not only in more high-tech equipment and effective medications but in more equitable social policies as well.